|
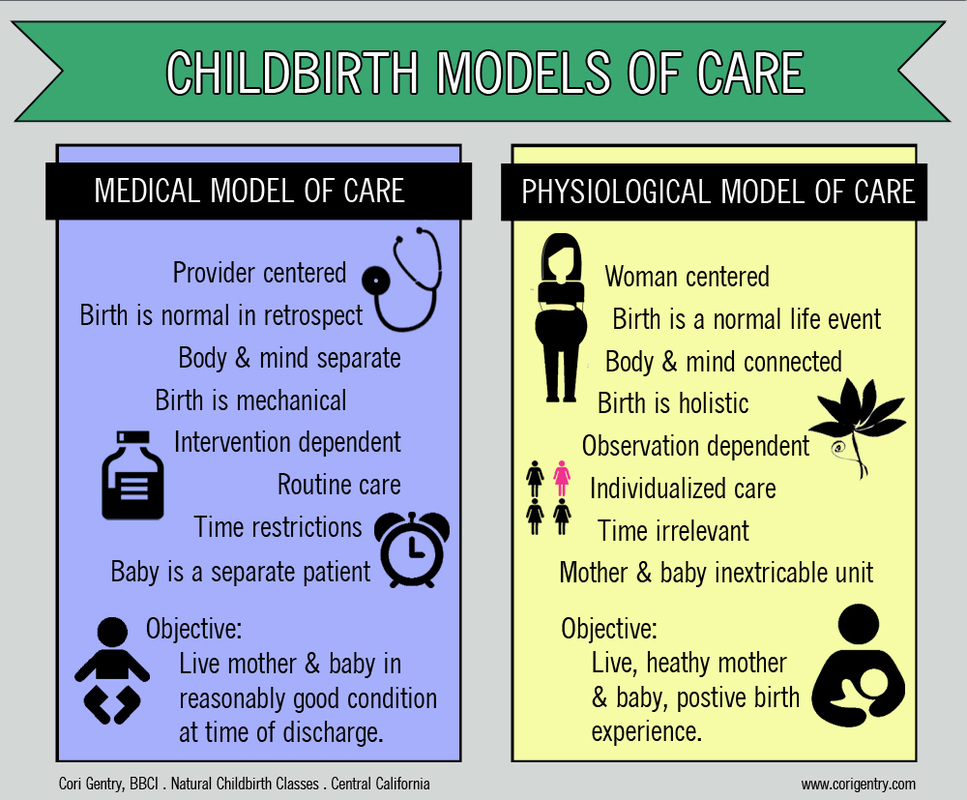
There are two approaches to maternity care: The medical model of care and the physiological model of care, also known as the midwifery model of care. Knowing the different maternity care models and which your provider practices can help you know what to expect during your pregnancy and birth and what your options are within that care model. The Medical Model of Care "Pregnancy in western society, in fact, straddles the boundary between illness and health" - Comaroff 1977: 116 The medical model of care (also known as the technocratic model of care or medical management) is a specific approach to maternity care that both doctors and midwives can subscribe to. If your care provider states that they follow the medical model of care, it's important to know what exactly that means. "Medical management practitioners start from the premise that pregnancy and birth are intrinsically difficult and potentially dangerous process that, when left to occur naturally, frequently result in poor outcomes." - Optimal Care in Childbirth by Henci Goer For care providers that practice the medical model of care pregnancy is a condition that depends upon treatment for a positive outcome. Interventions are necessary and superior to the natural/normal birth process. Some key characteristics of the medical model of care:
The basic premise is that birth is a mechanical process that depends only on "the powers, passage, and passenger" or the strength of contractions, the size of the pelvis, and the size of the baby. No other factors are considered such as the emotional state of the mother, her laboring position, or whether routine interventions are interfering with the labor process. The theory presents that any problem in labor is mechanical and the provider as the mechanic can correct the situation with a procedure or medication. All unwanted effects of interventions are treated with more interventions: "...when high-dose oxytocin infusion leads to nonreassuring fetal heart rate, the medical management model calls for IV fluid boluses, internal fetal monitoring, and, ultimately, cesarean surgery." Optimal Care in Childbirth by Henci Goer This is opposed to lowering the oxytocin dose or avoiding its use in the first place. It is important to emphasize that there is not much space for wiggle room in the medical model. Many providers do try to accommodate women's wishes, but it is a system that is not easily adjusted. For example, a woman who wants the freedom of movement in labor and then chooses a birth place where continuous monitoring is the norm may be thinking, "well, how hard is it to just not hook me up to a monitor?" Very. That monitor is apart of their staff. It reports to the nurses station so that one nurse can be assigned to several mothers. That nurse may not be able to effectively do her job without the monitor. Also, your care provider may be able to access the monitor readings from home or the office, which is a convenience that would be hard to give up. The monitor is also essential to the provider who believes birth is a runaway train ready to fly off the tracks at any moment. Without the monitor, how can a woman labor safely? Those taught under this theory literally may know of no other option. The monitor also reinforces the belief that the baby is a separate patient from the mother needing protection should the mother pursue her desire for a birth experience over the safety of her baby. Refusing an intervention in the medical model of care is not like asking for your burger with no pickles, it's a complicated system and an entire birth philosophy held dearly by its followers. The medical model calls for less time spent assessing the mother as an individual, making this approach convenient for providers. Most routine tests will pick up possible problems in the pregnancy, but at the cost of providing individualized preventative care. For example, instead of looking at a mother's risk factors, family history, and talking to her about nutrition and exercise in early pregnancy, a provider will routinely screen all women for gestational diabetes late late in pregnancy and then treat the women who develop the condition. Treatment may be hard on mom and prevention may have yielded better outcomes, but individualized care is unrealistic in busy practices that see lots of moms. If you are very comfortable with your care provider making decisions for you and you don't mind medical procedures being done even if they may not be necessary, then choosing a provider that follows the medical model will likely not conflict with your personal feelings about birth. If you would like to be apart of making decisions about your care, would prefer a low intervention birth, or believe that pregnancy and birth are a normal part of a woman's life, you will encounter more conflict in this model of care. The Physiological Model of Care “Remember this, for it is as true as true gets: Your body is not a lemon. You are not a machine. The Creator is not a careless mechanic. Human female bodies have the same potential to give birth well as aardvarks, lions, rhinoceri, elephants, moose, and water buffalo.” - Ina May Gaskin, Ina May's Guide to Childbirth The physiological model of care is more commonly referred to as the midwifery model of care, and sometimes woman-centered care. Physiological refers to a characteristic of an organism's healthy or normal functioning (Merriam-Webster Online). The belief held by followers of the physiological model of care is that birth is fundamentally healthy and normal and birth is safest when practices facilitate normal birth. The physiological model of care is a holistic approach that addresses a woman's physical, psychological and social well-being: "The midwifery model of care makes the woman and her life the central focus of prenatal care. A large part of the midwife’s attention focuses on the pregnant woman as a unique person, in the context of her family and her life. The midwife is interested in the woman’s expectations and experience of her pregnancy—her perceptions and beliefs; her knowledge and opinions; her questions and worries; her satisfactions and dissatisfactions; her comforts and discomforts; her desires, decisions, and actions; and the effect of all these on her pregnancy, fetus, labor, delivery, breastfeeding, postpartum recovery, and development as a mother." - Our Bodies Ourselves Some key characteristics of the physiological model of care:
Women who transfer from a provider practicing the medical model of care to one practicing the physiological model of care are often shocked by the differences. Appointments are longer and much more in depth. The provider following the physiological model of care will usually ask the mother what her wishes are in birth as apposed to a women having to ask if a provider will "let her" fulfill whatever her wishes are. Women are an active participant in their prenatal care. The physiological model of care supports autonomy between the provider and mother. In the medical model of care supports class distinctions where the provider holds I higher class standing than the patient. The physiological model of care recognizes that the couple is able to take responsibility for their birth and take part in the decisions that will affect it. Couples are often encouraged to research and care options are thoroughly explained. The woman is not caught in a system where the provider/institution may be biased towards a higher intervention birth which would yield more income for the provider/institution. Holding the perspective that birth is normal does not mean fewer precautions are taken in ensuring a healthy and happy mother and baby. While tests and procedures are not used indiscriminately, all of the tools (like doppler to listen to baby's heart beat, checking blood pressure, ordering blood tests and ultrasounds) employed by those practicing the medical model of care are still used in prenatal visits, but care is taken to ensure all tests are appropriate. The physiological model of care is most often adopted by midwives. While doctors are trained in seeking out complications and intervening in labor, with little or no training in normal birth, midwives receive extensive training in how to facilitate normal birth in addition to being able to identify complications so that mothers who need an obstetrician can receive that care. Middle Ground Model of Care Yes I made that up. Is there a place in maternity care for two models that appear to be so different? A 1999 study distributed a questionnaire to pregnant women regarding their provider style preferences. It found that women preferred elements of both midwifery and medical styles of care." Concluding that: "Broadening access to obstetric care will involve moving from our own preconceived notions of appropriate packaging into a patient-based and multi-option setting for delivery of these services." As women become more informed about our options and the differences between the medical model and physiological model of care many may switch from providers and hospitals that only offer the medical model for providers. This is a positive change for women, and hopefully a wake-up call to those individuals and institutions not practicing woman-centered, evidence-based care. However, hope is not lost for medicine! With cooperation from those who practice the medical model but want to give women options, there is room for both models in maternity care: "Midwifery and medical obstetrics are separate but complementary professions with different philosophies and overlapping but distinct purposes and bodies of knowledge. Physicians are experts in pathology and should have primary responsibility for the care of pregnant women who have recognized diseases or serious complications. Midwives are experts in normal pregnancy and in meeting the other needs of pregnant women— the needs that are not related to pathology. In most countries, midwives have primary responsibility for the care of women with uncomplicated pregnancies." - Our Bodies Ourselves In most of the rest of the developed world in countries like the United Kingdom, Australia, and Japan, low risk women see midwives while women who are determined to need an obstetrician transfer care to one. The result? These countries have much lower rates of maternal and infant deaths... in fact, we are rated 47th. It is safer to give birth in Singapore (3 deaths per 1000 births), Iceland (5/1000), and Qatar (7/1000) than it is to birth here (21/1000). Medicine plays an essential and irreplaceable role in our society, but the medical management model of care alone is an unbalanced system leaving few options for low risk women who hope to have an uncomplicated, normal birth. As an expecting couple you are the consumers. You have a choice in what kind of care you receive. More than just your birth experience rides on that decision.
0 Comments
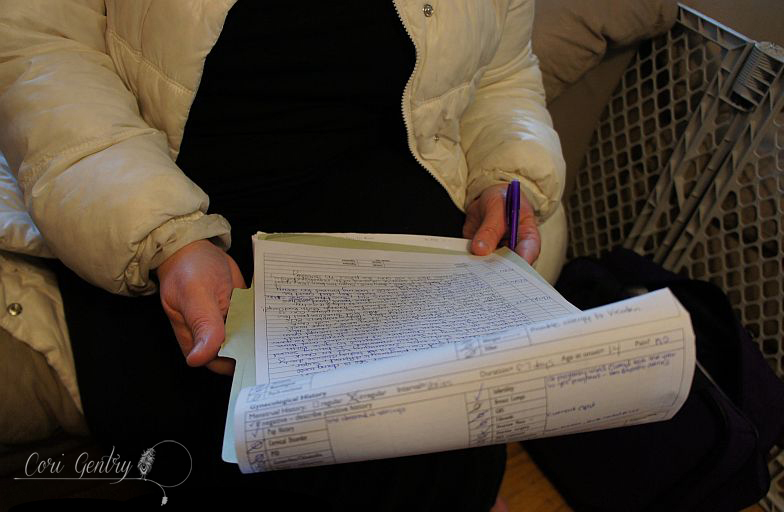
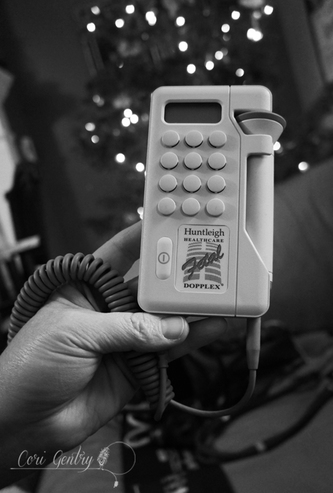
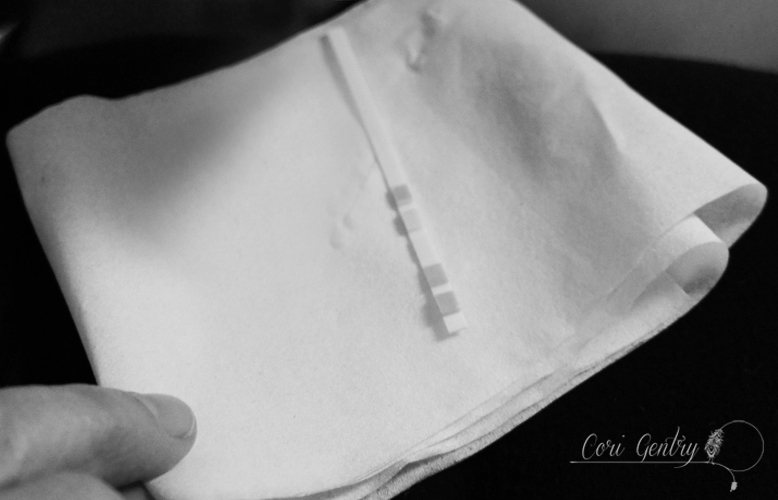
There is a segment in the birth documentary, The Business of Being Born, where an obstetrician is being interviewed about her opinions on midwifery care and homebirth. She says it scares her, and "can they even monitor a baby at home?" To those of us who are familiar with midwifery care, this is hilarious... and the answer is a resounding "of course!" However, with more than 90% of women never experiencing what prenatal care with a midwife is like, it's completely reasonable for people to be unaware of a midwife's capabilities and maybe have some reservations about the level of care they can even provide. I admit, the first midwife attended birth I heard about involved a cabin and a boiled shoelace. I was horrified, as I'm sure most modern women would be. I thought it might be fun to share with you what an appointment with my midwife, Jill, here in Salinas is like. People are usually shocked that my appointments typically run an hour, sometimes more if we get chatting. Some midwives work in offices alongside obstetricians, some work in birth centers (we don't have that option here either), some have their own offices where they conduct appointments and some come to the homes of their clients. That is what mine does, usually while my kids nap. Jill always begins with how I'm feeling and asks lots of questions about how I'm doing both physically and emotionally, which I appreciate since I have an awful memory and I often forget everything I wanted to ask if I get rushed. We talk about what I'm eating, what supplements I'm taking, and because I have gestational diabetes, we discuss my blood sugar levels over the last couple weeks which I've recorded for her. She takes down my weight and adds notes to my chart. Then Jill check's my blood pressure. It's usually perfect, better than usual for me actually, but if it's a bit high I lay down and we take it again... just in case. This is my favorite part of our appointment, and what I most miss when I see an obstetrician. Jill checks the position of baby by palpating my belly. I know that an OB can give me the same information with a quick ultrasound, which is why many OB's don't know how to palpate... but it's not the same. Baby was awake and very active this day but Jill finally cupped her hand near my ribs and said, "there... that's a little butt there," and near the left side of my pelvis, "and here's a head, baby is really having a good time in there wiggling around." Then Jill checks my fundal height, which is the length in centimeters from the top of the pelvis to the top of the uterus, or fundus. Every centimeter equals another week. We just want to make sure I'm growing. Here I'm 33 weeks, I measured 35. Baby feels like it's average sized but she could feel lots of fluid. My babies are typically well cushioned... and whoever is unfortunate enough to be in the splash zone when my water breaks usually needs a change of clothes. This one goes out to that OB in The Business of Being Born. Jill always brings her doppler, which allows her and anyone in the room to hear baby's heartbeat. While we have used it a few times, I usually ask her to use the fetoscope to minimize baby's exposure to ultrasound. After feeling where baby is Jill typically finds a heartbeat right away, and today was no different. The first time I saw a fetoscope I thought it was ridiculous looking, but it's specially designed to use the practitioner's forehead to conduct sound. I can't hear baby, but it's a worthwhile trade off to minimize exposure and risk to baby. My choice, Jill and many other midwives are happy to use the doppler too. Next I get my feet and ankles checked out for and signs of edema, or swelling, which could indicate problems related to gestational diabetes or preeclampsia. Thoroughly screening for any thing that may need medical attention is a huge part of our appointments and we always air on the side of caution. We do a urinalysis to check for protein, sugar, blood, ketones and leucocytes (white blood cells)... which tell Jill all kinds of stuff. Late in pregnancy protein may indicate preeclampsia. Protein can also indicate a urinary tract infection or a kidney issue. Sugar could indicate that the gestational diabetes is not being controlled. Ketones show up when the body burns fat instead of carbs and could mean I need to be eating more (never an issue... I eat a lot!). Leucocytes or bacteria would mean that there is an infection. I totally should have done my nails, that's not a weird happy face on my thumb nail, that's badly chipped polish. Jill checks my hemoglobin with a simple finger prick. Hemoglobin is a protein in the red blood cells that carry oxygen. Mine is a little low so I supplement with Floridex, a liquid iron supplement that I highly recommend to any mama with low iron.
We finish up with a drum circle and hallucinogenic herbs... ok not true... two people can't make a circle. An appointment with a midwife is really not that much different from seeing an obstetrician, you get all of the same important medical screening, plus added attention to how you are doing as a whole and a more hands on approach to care. I don't feel like I'm being examined as much as I feel like we are working together to make sure baby and I are healthy. |
 I'm a childbirth educator, birth doula, and birth activist with 4 little boys and occasionally enough time to write. I'm a childbirth educator, birth doula, and birth activist with 4 little boys and occasionally enough time to write.
EventsNatural Birth Series
Sept 28 – Nov 15 Carmel, 6:30–9pm Register Infant Sleep for Expecting & New Parents September 28th 6:30pm - 9:00pm Register Gentle Cesarean: Planning & Recovery September 30th Toro Park, 3-6:30pm Register Natural Birth Refresher October 15th Salinas, 1– 4pm Register Preconception & Early Pregnancy Class October 22nd Salinas, 1– 4pm Register Sibling Prep for Parents & Kids November 4th & 5th Toro Park, 2:-4pm Register Fall Home & Birth Center Birth Series Nov 7 – Dec 12 Salinas 7pm–9pm Register VBAC Class November 12th Salinas, 1–4pm Register Natural Birth Series Nov 29th – Jan 17th Salinas 6:30–9pm Register Archives
January 2017
Categories
All
|